Overview
The Pennsylvania Department of Education (PDE) oversees 500 public school districts, more than 170 public charter schools, public cyber charter schools, Career and Technology Centers/Vocational Technical schools, public Intermediate Units, the education of youth in State Juvenile Correctional Institutions, Head Starts and publicly funded preschools, and community colleges.
PDE also oversees policies related to public, academic, and school libraries, and the State Library of Pennsylvania.

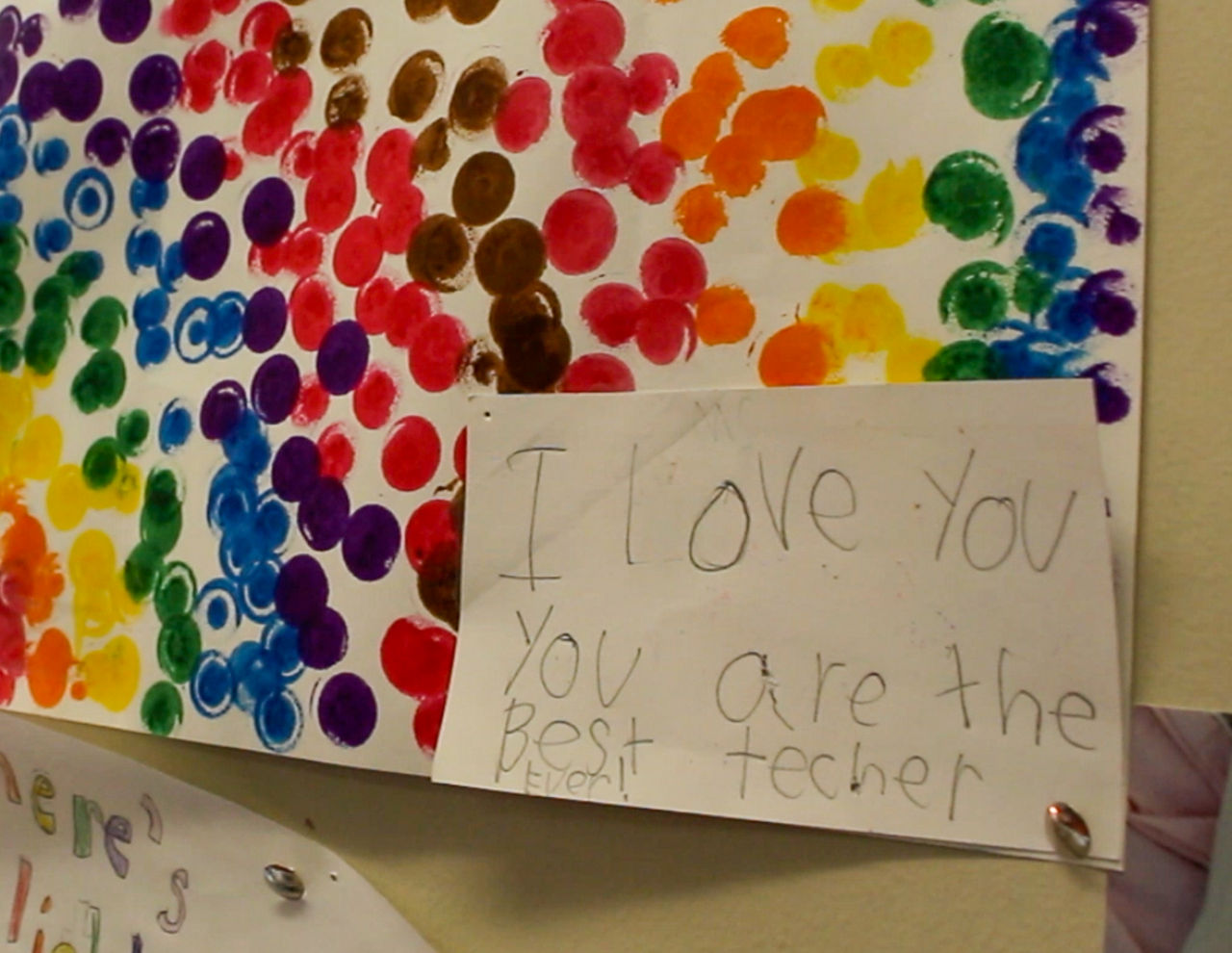
Teach in PA
More about Teach in PA (opens in a new tab)
Food & Nutrition
More about Food & Nutrition (opens in a new tab)
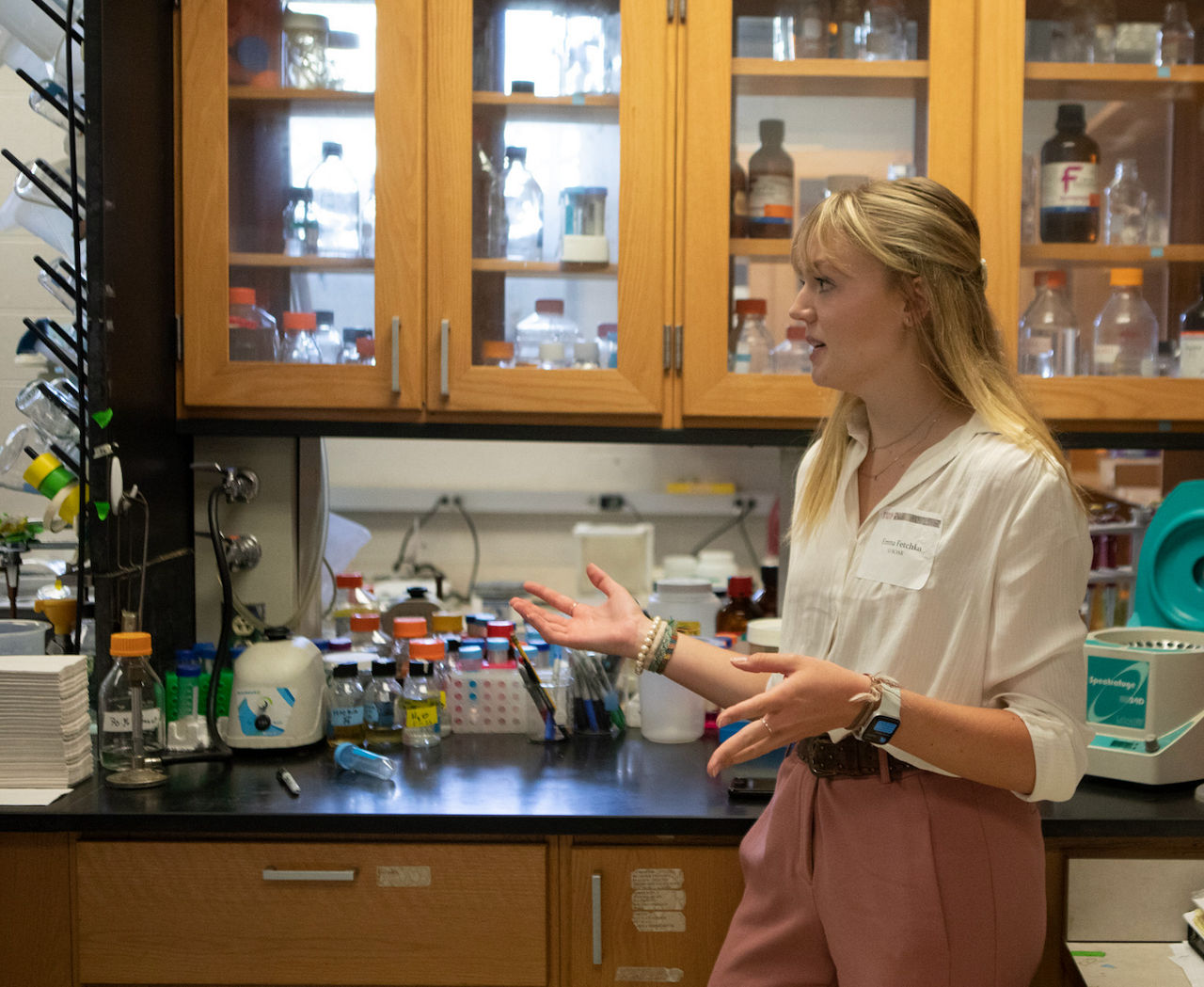
Career and Technical Education
More about Career and Technical Education (opens in a new tab)-
June 26, 2025 Pennsylvania Sees Boost in Certified Teachers as Shapiro Administration’s Educator Workforce Strategy Delivers Results
-
June 17, 2025 Shapiro Administration Highlights How Increased Funding for Career and Technical Education Helps More Students Gain Experience and Skills Critical to PA Workforce
-
June 13, 2025 Shapiro Administration Awards More Than $3.6 Million in Grant Funding to Support Family Literacy Across the Commonwealth
-
June 05, 2025 Shapiro Administration Ends Receivership for Harrisburg City School District
-
State Library of Pennsylvania Collecting, preserving, and providing access to materials for, by, and about Pennsylvania.
-
Professional Standards and Practices Commission The Professional Standards and Practices Commission sets preparation, certification, practice, and conduct standards for teachers.
-
State Board of Education The State Board of Education reviews, develops, and adopts regulations that govern basic and higher education in the Commonwealth.
-
State Board of Higher Education Provide direction, coordination, and support to ensure that institutions of higher education fully meet the workforce and economic development needs of this Commonwealth.